Before we start, please be advised that this article is only written for informative purposes and is not to be considered as a diagnostic tool or as a prescription for treatment.
Chronic obstructive pulmonary disease or COPD – as it is often referred to in the medical community is often caused by smoking, pollution, prolonged exposure to air pollution, genetic factors or infections contracted in early childhood.
Before we see the symptoms and its treatment, let us break down the name of the disease itself. Medically speaking, pulmonary means related to the lungs, obstructive would imply that something is blocking the airway or rather narrowing it down essentially leaving it almost closed and conditions or diseases are considered chronic when last for more than 3 months, usually with the condition needing continuous medication and its effect worsening over time. The chronic diseases do not have cures but can be managed with medication to improve the quality of life for the patient.
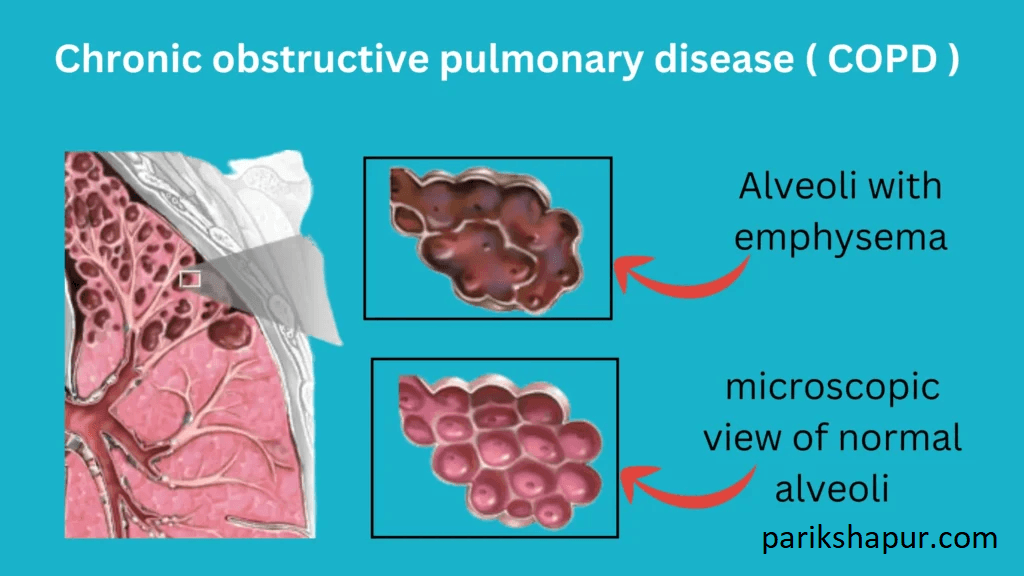
Let us see what COPD does to the body. Those looking for just the symptoms and treatment can skip this part and move on to the next paragraph. COPD is a lung disease, leaving it essential to understand the basic components of the lungs and how they work and contribute to its functioning. This pair of organs situated in the chest (thoracic region), are responsible for getting oxygen (O2) into the blood and filtering out carbon dioxide (CO2) from the blood. Consider each lung to be shaped like a cauliflower or a broccoli for analogical purposes. The bronchial tubes (airways) branch out the primary bronchia (like stems from the base) and they lead to bronchioles (smaller branches) that have alveoli (like the flowerets). The alveoli have blood vessels in them, that make the exchange of gases to and from the blood possible. The human lung is very expandable, in fact, its full size in adults can go up to 6 litres and the total area for air exchange is approximately 85 m2 (almost the size of a tennis court). In COPD, the airways (bronchia) are damaged due to inflammation. It also tears the air sacs (alveoli) and destroys it making it difficult for gas exchange to occur. The irritability from the smoke causes the body to produce more mucus and the inflammation also restricts the ability of the alveoli and bronchia to compress and decompress.
All of the above, trigger the patient to cough, produce excess phlegm (mucus), breathing difficulties, and wheezing for air during strenuous activities. Unfortunately, since the organ is capable of expanding a lot and has the ability to carry out its function even after considerable damage, it becomes difficult for the carrier/ patient to detect COPD in its earlier stages. More often than not, the carrier realises the threat of disease much later, after it becomes unmanageable by themselves. The disease progresses in 4 stages and the progression is measured FEV (Forced Exhale Volume). The FEV1, FEV2 and FEV3 are measured for every 1 second of forced exhale.
• Stage 1 COPD is a mild strain on the lungs, with the FEV1 measure being 80% or more of the pre-determined value. The patient feels a slight shortness of breath and dry cough present only while doing stressful physical work.
• Stage 2 COPD puts more strain on the lungs which is noticeable yet manageable in the patient. The FEV1 value is only 50% – 79% of what it should be. The patient presents a clear shortness in breath with a lot of coughing. They also would have some sputum (coughed up phlegm).
• Stage 3 COPD clearly presents in the patient with an exacerbation in symptoms. The FEV1 by now is only 30% – 49% of its predicted value.
• Stage 4 COPD is presented with less than 30% FEV1. The patient has laboured breath and wheezes often.
Apart from the lungs, COPD can also cause heart failure, lung cancer, thinning of bones (osteoporosis), collapsed lung, etc.
COPD can be managed with a wide range of medication, exercising or surgery. Please be advised, the treatments given here are in general and the patient presenting the symptoms needs to be treated and advised by a pulmonologist for any real betterment. There are breathing exercises, inhalation techniques that can improve the quality of breathing. Those with severe COPD may need surgery or oxygen therapy for the rest of their lives to be breathe properly. The patients in different stages may also need to take medication – for anti-inflammation (Phosphodiesterase 4 inhibitors), bronchodilators (beta-2 agonists, anticholinergics, arformoterol, formoterol), steroids (beclomethasone, ciclesonide, methylprednisolone, prednisone), antibiotics either short term or long term to manage their symptoms.
COPD can be managed by engaging in active rehabilitation. Practicing regular light sporting activities, getting the required emotional and mental support. If the patient is a smoker, there are programs that help in quitting the habit healthily. The patients can also get help in adjusting their routines, food habits and life style choices.